A University of Iowa Health Care study that links the location of a brain injury to levels of depression in patients following the injury has identified two distinct brain networks; one associated with increased depression symptoms and one associated with decreased depression symptoms.
The study expands on previous findings and suggests that these brain networks might be potential targets for neuromodulation therapies to treat depression.
Neuromodulation, also known as brain stimulation, is emerging as a tool to treat mood disorders. However, understanding which areas of the brain to target to get the best therapeutic effect is still limited, according to a press release.
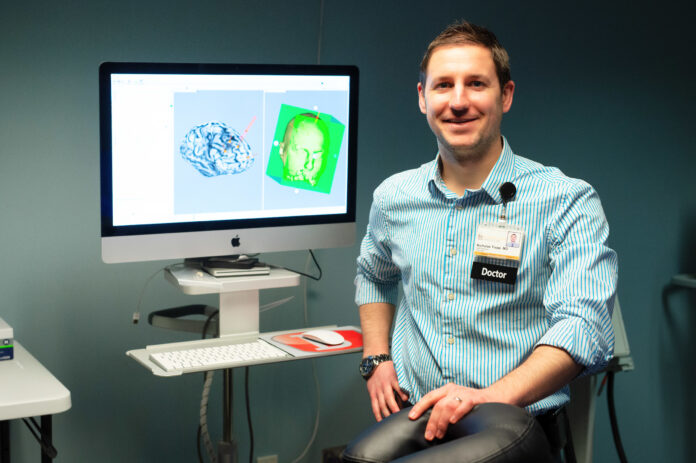
“We found some really interesting results identifying specific brain structures that were associated with higher levels of depression post lesion, and surprisingly, also found some areas that were associated with lower-than-average levels of depression post lesion,” says Nicholas Trapp, MD, UI assistant professor of psychiatry and lead author of the study, in a statement.
Regions most strongly associated with increased depression coincided with the nodes of the so-called salience network, which is involved in task reorientation, attention and emotion processing.
In contrast, peak resilience regions that were associated with less depression were part of a network known as the default mode network, which is thought to be involved in introspection, or self-referential thinking.
Patients whose brain lesions did not fall within either network had an average score of depression following their brain injury and provided a comparison group in the study.
Trapp hopes the findings will improve understanding of the causes of depression and potentially lead to better treatments.
“This could open the doors to potential studies looking at deep brain stimulation, or non-invasive forms of stimulation like TMS, where we might be able to modulate the specific brain areas or networks that we’ve identified, to try to get antidepressant effect, or potentially other therapeutic effects,” he said.
Published in the journal Brain, the findings used brain imaging scans and depression scores from 526 patients.
The study was funded in part by grants from the National Institute of Mental Health, the National Institute of Neurological Disorders and Stroke, and the Kiwanis Neuroscience Research Foundation.
More: UI research finds SPACs have less reliable financial reporting




